Daily Routines After Laryngectomy And How To Cope With The Changes
This short article describes the troubles laryngectomees face after partial or total laryngectomy. How To Cope With The Changes?
Life undergoes significant changes following a total or partial laryngectomy, primarily due to the lasting effects of radiation and surgery.
Radiation therapy can lead to muscle fibrosis in the jaw, resulting in difficulties in opening the mouth (trismus or lockjaw), making eating more challenging. Reduced saliva production, narrowing of the esophagus, and a lack of peristalsis in individuals with flap reconstruction can also contribute to eating and swallowing difficulties. Additionally, the ability to smell is affected as air inhalation bypasses the nose.
Smelling after laryngectomy
Laryngectomees might experience problems with their sense of odor. This is despite the fact that regular laryngectomy surgical treatment does not include nerves related to the sense of odor and the sense of smell, or olfaction, remains intact.
What has altered, nevertheless, is the pathway of air flow throughout respiration. Prior to a laryngectomy, air flows into the lungs through the nose and mouth. This movement of air through the nose allows for aromas and scents to be detected as they come in contact with the nerve endings in the nose responsible for the sense of odor.
Laryngectomees may encounter challenges with their sense of smell, despite the fact that standard laryngectomy surgery does not affect the nerves responsible for olfaction, or the sense of smell, which remains intact.
However, the alteration lies in the airflow pathway during respiration. Prior to laryngectomy, air entered the lungs through the nose and mouth. This nasal airflow allowed odors to be detected as they interacted with the nerve endings responsible for smell in the nose.
Difficulties in breathing and defecation due to changes in airflow affect the acceptance of disability post-laryngectomy. Therefore, nurses must meticulously assess daily life challenges and the patient’s ability to perform self-care activities such as breathing and defecation to facilitate acceptance of disability and aid in adaptation to life after total laryngectomy.

Challenges in breathing and defecation resulting from a permanent tracheal stoma hinder the acceptance of disability, with acceptance associated with difficulties in these functions. Self-assessment of functional impairment and daily activities post-laryngectomy empowers patients to adapt to lifestyle changes and fosters a sense of control, increasing self-efficacy.
Moreover, patients regain confidence by managing physical issues and everyday challenges, leading to awareness of positive changes and increased satisfaction in postoperative life, promoting self-acceptance.
Therefore, nurses should thoroughly assess daily life issues, promote self-care of the tracheal stoma, provide education, and offer continuous support to enhance self-care capabilities and life satisfaction post-discharge.
Regular nursing support through home visits and outpatient services can heighten patients’ sense of control over daily life challenges and foster positive acceptance of disability, facilitating adjustment to life after laryngectomy.
Irregularity decreases the quality after laryngectomy.
Although laryngectomized patients often experience constipation as a significant issue, they tend not to communicate this concern to healthcare providers due to insufficient awareness of its importance.
Functional constipation appears to be more prevalent among laryngectomized patients, particularly those over the age of 65, compared to non-laryngectomized individuals under 65. Factors contributing to this risk after surgery include age, dietary changes, altered defecation habits, anxiety, immobility, and lack of glottic closure.
However, patients frequently fail to recognize these contributing factors.
Narrowing of the esophagus and swallowing issues
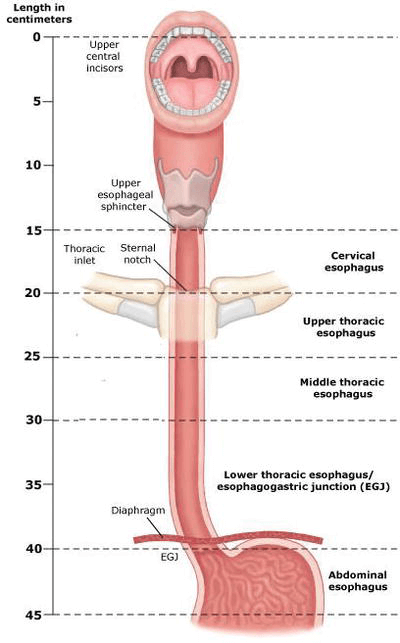
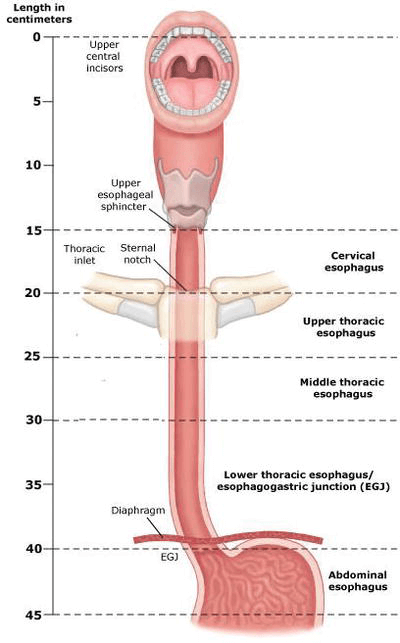
A stricture of the esophagus is a narrowing along the pharyngo-esophagus that blocks or prevents the ease of food passage, leading to the esophagus having an hour-glass setup.
Strictures after laryngectomy can be due to the results of radiation and the tightness of the surgical closure and can likewise develop slowly as scarring forms.
Interventions that can help the patient consist of:
- Postural or dietary changes
- Myotomy (cutting the muscle).
- Dilatation (see listed below).
The free flap commonly used in larynx replacement surgery lacks peristalsis, making swallowing more challenging. Following surgery, food descends to the stomach primarily by gravity, with the time taken varying between individuals, typically ranging from 5 to 10 seconds.
To aid swallowing, it is helpful to chew food thoroughly and mix it with liquid before swallowing, taking small amounts of food at a time and allowing it to go down. Drinking liquids between solid foods can help flush down the food.
Eating may take longer, requiring patience to finish the meal. Swelling immediately after surgery gradually decreases over time, reducing constriction of the esophagus and easing swallowing.
While there is hope that swallowing difficulties will diminish within the first few months after surgery, if they persist, esophageal dilation is one therapeutic option to consider.
How To Cope With The Changes: take care of yourself
How To Cope With The Changes: Activity.

Rest when you feel exhausted. Getting enough sleep will help you recuperate.
- Sleep with your direction by using 3 or four pillows. You can also attempt to sleep with your direct in a reclining chair. Do not sleep on your stomach.
- Try to stroll each day. Start by strolling a little more than you did the day previously. Bit by bit, increase the amount you walk. Walking increases blood flow and helps prevent pneumonia and irregularity. You might climb up stairs.
- If you have a stoma in your neck, be mindful while showering and shaving. Do not get water in the stoma, because it might enter your lungs. If you have a stoma, follow your physician’s instructions on how to care for it.
- Do not lean your head back rapidly or for a very long time. This puts pressure on your neck and might slow your recovery.
- Avoid strenuous activities, such as bike riding, jogging, weight lifting, or aerobic workout, up until your physician says it is fine. This consists of cutting the yard or shovelling snow.
- For about 6 weeks, prevent raising anything that would make you strain. This might include a kid, heavy grocery bags and milk containers, a heavy brief-case or knapsack, cat litter or dog food bags, or a vacuum.
Ask your doctor when you can drive once again.
How To Cope With The Changes: Diet.

Typically, the transition takes 1 to 2 months, during which your physician will provide specific dietary instructions.
If you’re on a soft diet, focus on easily digestible and swallowable foods such as waffles, pancakes, most cereals, scrambled eggs, canned fruits, tender meats (hamburger, turkey, chicken, pork), mild cheeses, potatoes, pasta, and cooked vegetables. Maintaining weight and energy is crucial, so avoid filling up on sweets like candy and cookies, as they may lead to lightheadedness and a condition called dumping syndrome, characterized by faintness, bloating, shakiness, nausea, and diarrhea.
To aid digestion, stand upright during meals and for 30 to 60 minutes afterward. Avoid eating anything within 3 hours of bedtime. Consider taking a daily fiber supplement to promote regular bowel movements. If you haven’t had a bowel movement in a few days, consult your doctor about using a mild laxative.
How To Cope With The Changes: Other directions.
Here are some tips for caring for your stoma:
- Keep it covered with a light cloth to prevent dust and particles from entering your lungs.
- Consider using a humidifier to maintain moisture and prevent drying and crusting of the stoma.
- It’s normal to have some yellow-colored mucus around your feeding tube; this is not a sign of infection. Keep the feeding tube secured to your skin at all times with tape, ensuring there’s some slack to prevent accidental dislodging.
- If you’re unable to speak after surgery, a speech therapist will teach you alternative communication methods.
- Seek support from a counselor if you’re struggling to cope after surgery.
Acceptance of disability after laryngectomy is linked to difficulties in defecation and breathing. Nurses play a vital role in providing appropriate evaluations and interventions to help patients develop necessary self-care skills to manage daily life challenges. It’s important for nurses to support patients in coping with daily life issues, fostering positive acceptance of disability, and facilitating adjustment to life after laryngectomy.
See some of our Stoma Care Products and Labex Electrolarynx Devices!
Please consider joining our Labex Support Center for Laryngectomee FB group:.
https://www.facebook.com/groups/801546370394224.